
Why are you always hungry?
To better answer this question, it’s probably best to have a basic understanding of how you get hungry. Note: The information below comes from The Academy and it’s a simplified …
Read More
To better answer this question, it’s probably best to have a basic understanding of how you get hungry. Note: The information below comes from The Academy and it’s a simplified …
Read More
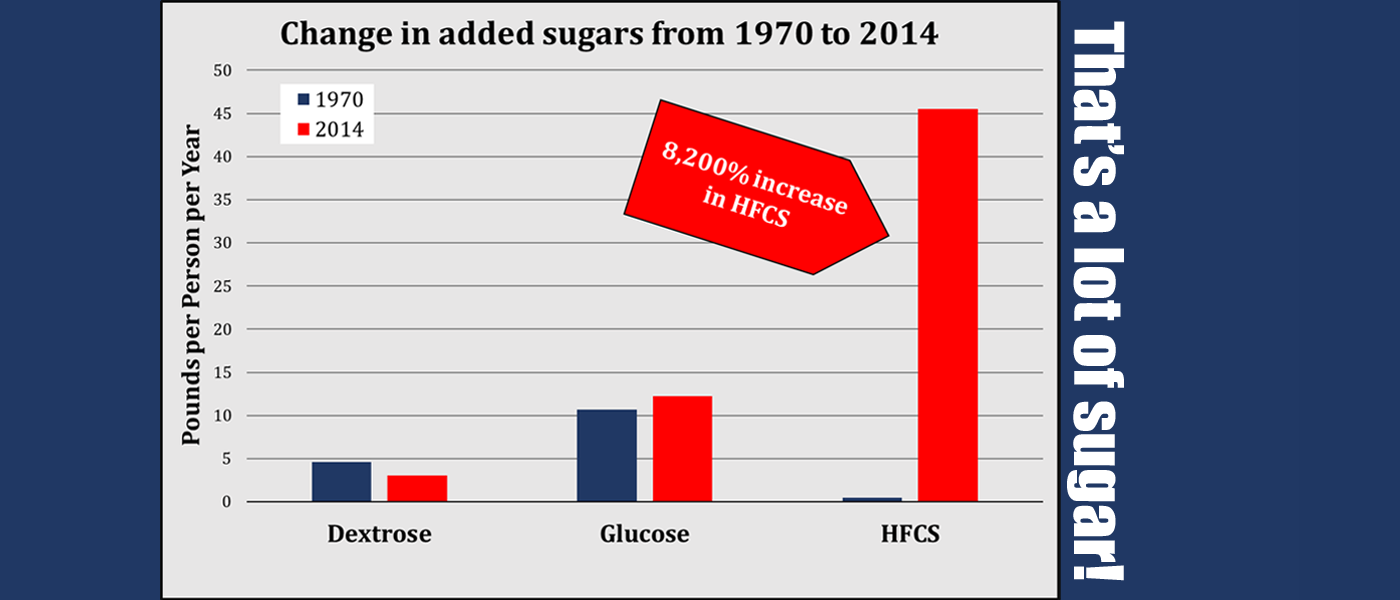
Would you like to know why our chronic disease problem is so bad? Look no further than this! The USDA recently published “U.S. Trends in Food Availability and a Dietary …
Read More
3 Snacks Type 2 Diabetics need to keep with them at ALL times! No blood sugar impact snacks Most type 2 diabetics struggle with controlling their blood sugar. Since almost …
Read MoreThank you for viewing our webinar! Listed below are links where you can download the files discussed during the webinar – the exercise tip sheet and the Module 1 Guide. …
Read More
What they aren’t telling you! As a type 2 diabetic, you are keenly aware of the importance in controlling your blood sugar. Whether it is with your diet, the frequency …
Read MoreWhat happens to the carbohydrates we eat? Type 2 diabetics (and many others) know they turn into blood sugar. Monitoring blood sugar is something a type 2 diabetic does daily. …
Read More
You’ve heard it before, maybe even believe it yourself: “Eat the egg whites and trash the yolks!” “Egg yolks are full of saturated fat and cholesterol – they are bad …
Read More
Dinner with the husband, the shakes and metabolic flexibility Have you ever experienced your hands starting to shake a little when you are hungry? When that happens, it’s time to …
Read More