
10X Your Disease Management and Wellness Program Engagement
How to 10X Your Disease Management and Wellness Program Engagement If you are lucky to get 10% engagement, then continue reading Why we do what we do If you …
Read More
How to 10X Your Disease Management and Wellness Program Engagement If you are lucky to get 10% engagement, then continue reading Why we do what we do If you …
Read More
The Health Performance Institute (HPI) is proud to announce that we are supporting the Tour de Cure this year. What is the Tour de Cure It’s the largest annual …
Read More
The OGTT (Oral Glucose Tolerance Test) is a good test when other methods for diagnosing type 2 diabetes are not available. It’s what comes after the test that is insane. …
Read More
To better answer this question, it’s probably best to have a basic understanding of how you get hungry. Note: The information below comes from The Academy and it’s a simplified …
Read More
Note: Cross-posted from Briansekula.com. The scientific literature has well-established the association between a lack of sleep and health-related issues. Basically, sleep deprivation is associated with every chronic condition on the …
Read More
Is type 2 diabetes forever? It’s what type 2 diabetics are told from the time they are diagnosed. For too many, the answer is yes. The answer can also be …
Read More
4 Things Type 2 Diabetics Must Do To Improve Insulin Sensitivity! Recently, Brian hosted a live video on the HPI Facebook page. He discussed why it is important for type …
Read More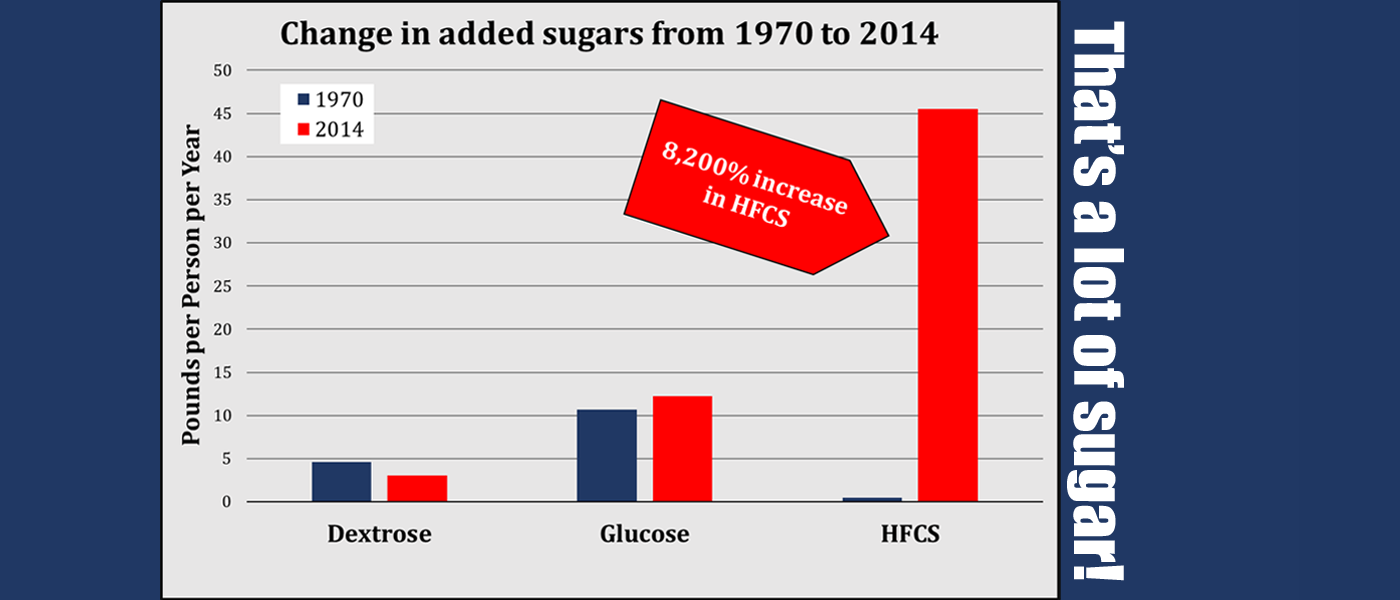
Would you like to know why our chronic disease problem is so bad? Look no further than this! The USDA recently published “U.S. Trends in Food Availability and a Dietary …
Read More
That’s it – 2 minutes. After a great weekend and time spent on Sunday prepping for Monday, I was ready. Around 5:30am, this is sitting at the top of my …
Read More